Abstract
Research Article
Shoulder muscle weakness effects on muscle hardness around the shoulder joint and scapulae
Kubota Atsushi*, Takayanagi Chiho and Kishimoto Kohei
Published: 21 April, 2020 | Volume 5 - Issue 1 | Pages: 001-007
Purpose: The time course of muscle stiffness of muscles around the shoulder joint and the scapula was investigated according to the degree of muscle weakness. This study was conducted to clarify the recovery process of muscle hardness of the muscles surrounding the shoulder joint and the scapula after the shoulder internal and external rotational exercises.
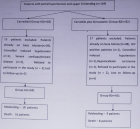
Methods: Participants were 7 healthy men (23.6 ± 1.4 yr), repeated internal and external rotations of the shoulder joint until the mean work of three internal and external rotations each was less than 90%, 80%, or 70% of the standard. Muscle hardness of the supraspinatus muscle, the infraspinatus muscle, and the rhomboideus muscle was measured before, immediately after, and 1to 72 hr after each bout of exercise.
Muscle hardness was measured as Strain ratio using an ultrasound real-time tissue elastography. In addition, the rates of change were calculated using muscle hardness before exercise as the standard, to compare differences in the rate of change after exercise between conditions.
Results: The rates of change of the Strain ratio between measurements taken before and after exercise were compared among conditions for the infraspinatus muscle. Results were -7.1 ± 5.3, -15.2 ± 10.3, and -25.0 ± 8.8, respectively, at 90%, 80%, and 70%, with a significant difference between a decrease to 90% and to 70% (p < 0.05). Significant difference was found in the change over time for the infraspinatus muscle only between values obtained immediately after exercise and after 72 hr at a decrease to 70% (p < 0.05).
Conclusion: Those results described above demonstrated that the infraspinatus muscle and the supraspinatus muscle were harder immediately after exercise when the shoulder joint was at a higher degree of muscle weakness, and demonstrated that the change was likely to be recovered after 72 hr.
Read Full Article HTML DOI: 10.29328/journal.jsmt.1001049 Cite this Article Read Full Article PDF
Keywords:
Baseball shoulder; Elastography; Internal and external rotation; Conditioning
References
- Baltaci G, Johnson R, Kohi H 3rd. Shoulder range of motion characteristics in collegiate baseball players. J Sports Med Phys Fitness. 2001; 41: 236-242. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11447368
- Oliver GD, Weimar WH. Hip and Shoulder Range of Motion in Youth Baseball Pitchers. J Strength Cond Res. 2016; 30: 2823-2827. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25486297
- Crockett HC, Gross LB, Wilk KE, Schwartz ML, Reed J, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002; 30: 20-26. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11798991
- Amin NH, Ryan J, Fening SD, Soloff L, Schickendantz MS, et al. The Relationship Between Glenohumeral Internal Rotation Deficits, Total Range of Motion, and Shoulder Strength in Professional Baseball Pitchers. J Am Acad Orthop Surg. 2015; 23: 789-796. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26609146
- Laudner KG, Wilson JT, Meister K. Elbow isokinetic strength characteristics among collegiate baseball players. Phys Ther Sport. 2012; 13: 97-100. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22498150
- Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006; 34: 385-391. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16303877
- Chou PP, Chou YL, Wang YS, Wang RT, Lin HT. Effects of glenohumeral internal rotation deficit on baseball pitching among pitchers og different ages. J Shoulder Elbow Surg. 2018; 27: 599-605. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29241660
- Tyler TF, Mullaney MJ, Mirabella MR, Nicholas SJ, McHugh MP. Risk Factors for Shoulder and Elbow Injuries in High School Baseball Pitchers: The Role of Preseason Strength and Range of Motion. Am J Sports Med. 2014; 42: 1993-1999. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24893778
- Bailey LB, Shanley E, Hawkins R, Beattie PF, Fritz S, et al. Mechanisms of Shoulder Range of Motion Deficits in Asymptomatic Baseball Players. Am J Sports Med. 2015; 43: 2783-2793. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26403207
- Takenaga T, Sugimoto K, Goto H, Nozaki M, Fukuyoshi M, et al. Posterior Shoulder Capsules Are Thicker and Stiffer in the Throwing Shoulders of Healthy College Baseball Players: A Quantitative Assessment Using Shear-Wave Ultrasound Elastography. Am J Sports Med. 2015; 43: 2935-2942. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26473012
- Byram IR, Bushnell BD, Dugger K, Charron K, Harrell FE Jr, et al. Preseason shoulder strength measurements in professional baseball pitchers: identifying players at risk for injury. Am J Sports Med. 2010; 38: 1375-1382. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20489215
- Trakis JE, McHugh MP, Caracciolo PA, Busciacco L, Mullaney M, et al. Muscle strength and range of motion in adolescent pitchers with throwing-related pain: implications for injury prevention. Am J Sports Med. 2008; 36: 2173-2178. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18596197
- Clarsen B, Bahr R, Andersson SH, Munk R, Myklebust G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: a prospective cohort study. Br J Sports Med. 2014; 48: 1327-1333. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24948083
- Moreno-Pérez V, Elvira J, Fernandez-Fernandez J, Vera-Garcia FJ. A comparative study of passive shoulder rotation range of motion, isometric rotation strength and serve speed between elite tennis players with and without history of shoulder pain. Int J Sports Phys Ther. 2018; 13: 39-49. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29484240
- Kusano K, Nishishita S, Nakamura M, Tanaka H, Umehara J, et al. Acute effect and time course of extension and internal rotation stretching of the shoulder on infraspinatus muscle hardness. J Shoulder Elbow Surg. 2017; 26: 1782-1788. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28684232
- Nordez A, Guével A, Casari P, Catheline S, Cornu C. Assessment of muscle hardness changes induced by a submaximal fatiguing isometric contraction. J Electromyogr Kinesiol. 2009; 19: 484-491. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18158253
- Yanagisawa O, Niitsu M, Kurihara T, Fukubayashi T. Evaluation of human muscle hardness after dynamic exercise with ultrasound real-time tissue elastography: a feasibility study. Clin Radiol. 2011; 66: 815-819. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21529793
- Kishimoto K, Sakuraba K, Kubota A, Fujita S. The effect of concentric and eccentric exercise on muscle hardness. Juntendo Medical Journal. 2018; 64: 371-378.
- Murayama M, Nosaka K, Yoneda T, Minamitani K. Changes in hardness of the human elbow flexor muscles after eccentric exercise. Eur J Appl Physiol. 2000; 82: 361-367. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10985588
- Howell JN, Chleboun G, Conatser R. Muscle stiffness, strength loss, swelling and soreness following exercise-induced injury in humans. J Physiol. 1993; 464: 183-196. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8229798
- Green MA, Sinkus R, Gandevia SC, Herbert RD, Bilston LE. Measuring changes in muscle stiffness after eccentric exercise using elastography. NMR Biomed. 2012; 25: 852-858. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22246866
- Lacourpaille L, Nordez A, Hug F, Couturier A, Dibie C, et al. Time-course effect of exercise-induced muscle damage on localized muscle mechanical properties assessed using elastography. Acta Physiol (Oxf). 2014; 211: 135-146. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24602146
- Proske U, Allen TJ. Damage to skeletal muscle from eccentric exercise. Exerc Sport Sci Rev. 2005; 33: 98-104. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15821431
- Peake J, Nosaka K, Suzuki K. Characterization of inflammatory responses to eccentric exercise in humans. Exerc Immunol Rev. 2005; 11: 64-85. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16385845
- Peake JM, Neubauer O, Della Gatta PA, Nosaka K. Muscle damage and inflammation during recovery from exercise. J Appl Physiol. 2017; 122: 559-570. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28035017
Figures:
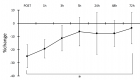
Figure 1

Figure 2
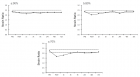
Figure 3

Figure 4
Similar Articles
-
Shoulder muscle weakness effects on muscle hardness around the shoulder joint and scapulaeKubota Atsushi*,Takayanagi Chiho,Kishimoto Kohei. Shoulder muscle weakness effects on muscle hardness around the shoulder joint and scapulae. . 2020 doi: 10.29328/journal.jsmt.1001049; 5: 001-007
Recently Viewed
-
Trends in TeledentistryRudrakshi C*. Trends in Teledentistry. J Clin Adv Dent. 2020: doi: 10.29328/journal.jcad.1001014; 4: 004-005
-
Au26-35: A Special Geometrical Structure of Au33 (D2) Cluster with Highly Occupied - 14 Pairs of Double-State DegeneracyK Vishwanathan*. Au26-35: A Special Geometrical Structure of Au33 (D2) Cluster with Highly Occupied - 14 Pairs of Double-State Degeneracy. Ann Adv Chem. 2022: doi: 10.29328/journal.aac.1001035; 6: 063-080
-
Texture of Thin Films of Aluminum Nitride Produced by Magnetron SputteringStrunin Vladimir Ivanovich,Baranova Larisa Vasilievna*,Baisova Bibigul Tulegenovna. Texture of Thin Films of Aluminum Nitride Produced by Magnetron Sputtering. Int J Phys Res Appl. 2025: doi: 10.29328/journal.ijpra.1001106; 8: 013-016
-
Minimising Carbon Footprint in Anaesthesia PracticeNisha Gandhi and Abinav Sarvesh SPS*. Minimising Carbon Footprint in Anaesthesia Practice. Int J Clin Anesth Res. 2024: doi: 10.29328/journal.ijcar.1001025; 8: 005-007
-
On Friedman equation, quadratic laws and the geometry of our universeS Kalimuthu*. On Friedman equation, quadratic laws and the geometry of our universe. Int J Phys Res Appl. 2021: doi: 10.29328/journal.ijpra.1001041; 4: 048-050
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."